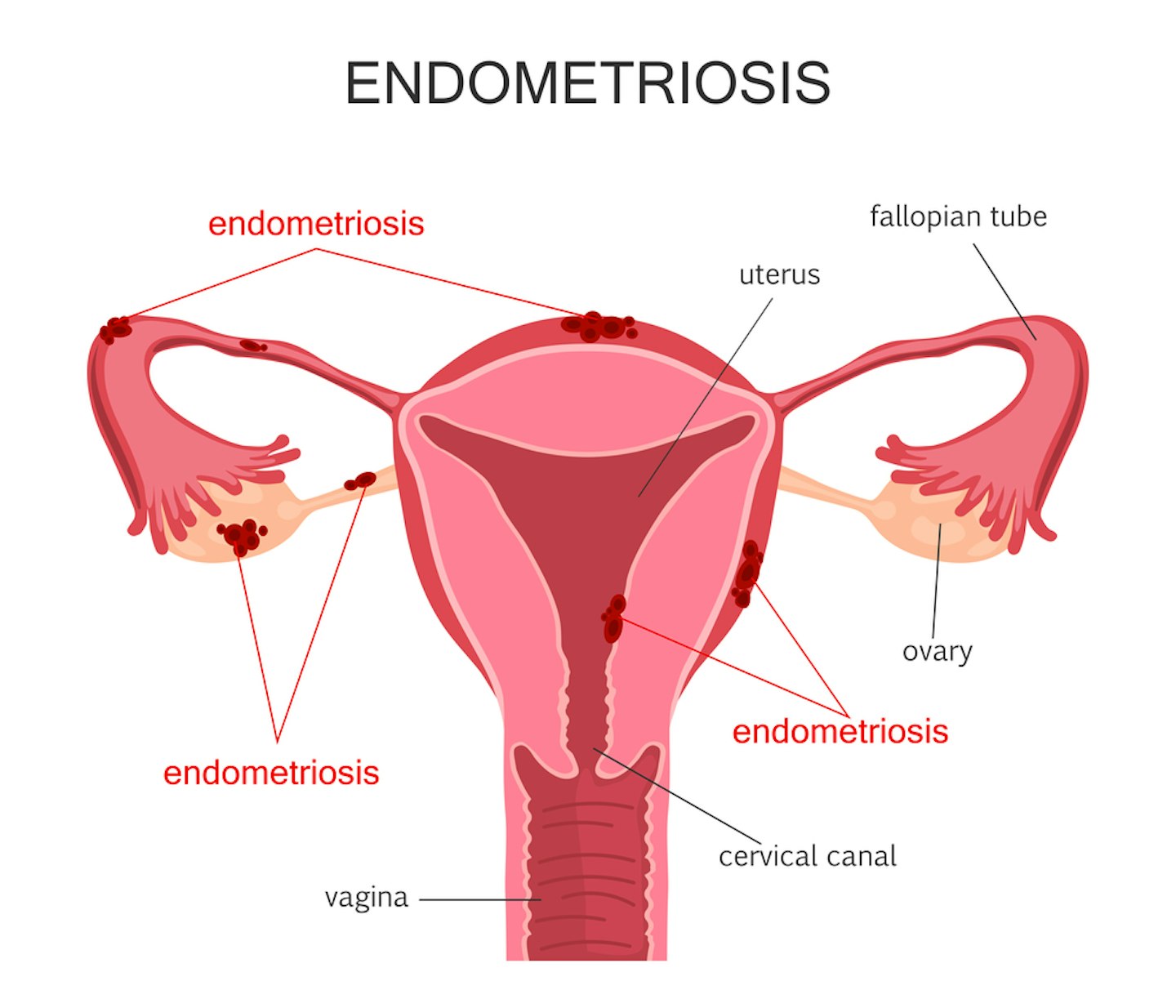
Endometriosis is a condition where cells, like those found in the lining of the womb, are found elsewhere in the body, such as the ovaries and fallopian tubes. It affects 1.5 million women and those assigned female at birth in the UK - that’s 1 in 10 women of reproductive age.
Endometriosis symptoms can cause great pain and discomfort for women, particularly during periods (dysmenorrhoea) and intercourse, and can also cause bowel, bladder, and fertility issues as it can be a sign you can't get pregnant. But what are the causes? And can it be cured?
Endometriosis Action Month
Every March, people around the world come together to support Endometriosis Action Month. It is an opportunity to raise awareness for the 1 in 10 women and those assigned female at birth with endometriosis, and campaign for more research to improve treatment and management options.
This month highlights the real impact of living with endometriosis – shining a light on areas including mental health, finances, soaring gynecology waiting times, and to ensure that all those with endometriosis have access to the right support at the right time.
The charity, Endometriosis UK will be hosting events and webinars throughout March for Endometriosis Action Month 2025.
What are the symptoms of endometriosis?
According to NHS guidance, the main symptoms of endometriosis are:
• Pain in your lower tummy or back (pelvic pain) including cramps – usually worse during your period
• Extreme period pain that stops you doing your daily activities
• Very heavy periods (bleeding through tampons and pads)
• Pain during or after sex
• Pain when peeing or pooing during your period
• Feeling sick, constipation, diarrhoea, or blood in your pee during your period
• Difficulty getting pregnant
It's also wise to be aware of the uncommon symptoms of endometriosis too as well as the difference between endometriosis vs adenomyosis.
What causes endometriosis?
Little is known about the causes, but some medical professionals believe genetics has a big part to play as well as retrograde menstruation, where the womb lining flows up towards the fallopian tubes instead of leaving the body as a period, and immune system weakness.
How is endometriosis diagnosed?
If you experience heavy or painful periods, or have been experiencing issues with fertility, it is worth talking to your GP about your symptoms and exploring the possibility of endometriosis being the cause.
Your doctor may examine your tummy and vagina and you may be referred to a gynaecologist for further tests. Ultrasounds can be used to diagnose endometriosis, but a procedure called a laparoscopy (where a camera is passed through a small cut in your tummy) is the only way to confirm if you have endometriosis.
For this reason, it can be difficult to diagnose endometriosis, and it can sometimes be confused with similar conditions such as adenomyosis, fibroids, pelvic inflammatory disease and irritable bowel syndrome.
Are there any treatments for endometriosis?
There are a wide range of treatments available for endometriosis, which can vary depending on the patient. These include age, patient priorities (e.g. pain/fertility), previous treatment history and so on. The severity of the condition can also dictate the treatment – for example, if a woman is approaching menopause, the symptoms of endometriosis may improve without treatment.
Pain management
Medications such as painkillers and anti-inflammatories can be prescribed to help patients manage pain. The impact of this pain on normal quality of life is often misunderstood, and it can greatly impact a woman’s ability to lead a normal life, also impacting their mental health.
Hormone treatment
Hormone treatments such as the combined contraceptive pill can be used to stop the growth of endometriosis tissue, and they work by mimicking pregnancy (when the endometrium, also known as the lining of the womb, is thin or inactive) or menopause (when the ovaries are inactive, and oestrogen is no longer produced).
Male hormones can also be prescribed as they help to lower oestrogen levels, causing the growth of the endometrium to stop. However, these hormones do come with many side effects and it is important to consider this when looking into treatment with your GP. Women seeking to conceive must place careful consideration on the impact of chronic hormone therapy on their desire to have a child.
Surgery
A surgical procedure called a laparoscopy (or keyhole surgery) can be performed to either excise the endometriosis by cutting out the clusters of cells implanted on other tissue; or they can treat it with electrical devices producing heat or laser. Laparoscopic surgery is effective, but this doesn’t mean the endometriosis won’t reoccur – there is still a chance of this. A surgeon must be skilled and be sure to treat the disease more completely to reduce the risk of recurrence.
Radical surgery - hysterectomy (removal of the womb) and/or oophorectomy (removal of the ovaries) – are other options, although these procedures are irreversible, and therefore require a great deal of consideration. Again, the desire to have a baby will play a role in selecting this therapy.
Endometriosis support
If endometriosis symptoms are taking their toll on your mental health, it's important to mention this to your GP and they may be able to help advise you and point you in the best direction for pain management and mental health care.
We've also put together some useful contacts and helplines if you need to talk to someone about how you're feeling.
About the author
Lorna White is the Products Editor for Mother&Baby. After running the Yours magazine website, specialising in content about caring for kids and grandchildren, Lorna brought her expertise to Mother&Baby in 2020. She has a keen interest in a range of topics from potty training and nutrition to baby names and early development and has a wide range of experienced medical experts and professionals at her fingertips. In her spare time, she enjoys spending time with her two young sisters, dog walking and enjoying the outdoors with her family.
